During the COVID-19 pandemic, local emergency management officials have referred to the local Local Health Authority in relation of positive patients. While many know that the LHA is involved during the COVID-19 pandemic, not everyone knows or understands the LHA’s role.
The Local Health Authority is appointed by the county government to provide support services in the absence of a county health department. Dr. I.L. Balkcom IV has served as Hopkins County’s LHA in the absence of a state health department for a number of years. Hopkins County Commissioners Court reappointed Balkcom on March 26 as the LHA.
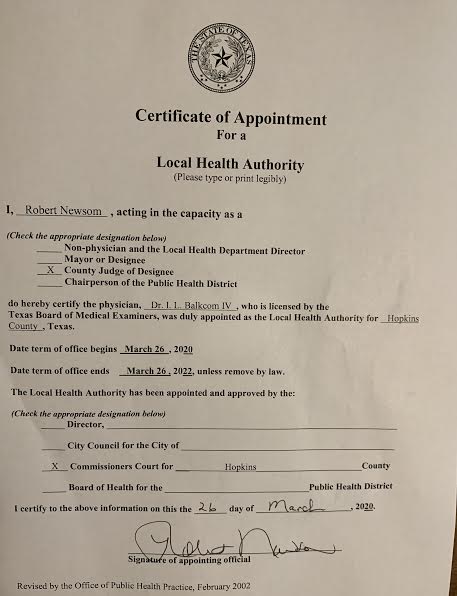
According to Texas Department of State Health Services, a Health Authority administers state and local laws relating to public health and local laws relating to public health within a local government’s jurisdiction.
LHA Patient Contacts, Tracing
During the COVID-19 pandemic, the LHA primarily helps with tracing not being conducted by the state and serves as a resource for patients and families who are under quarantine, if needed.
According to a LHA nurse, while the LHA may contact patients while they are in quarantine, that does not mean daily phone calls or screenings or that all patients will receive a call from the LHA.
Many patients are under the care of a physician who knows the patient’s medical history and needs or the patient has enough medical knowledge that it’s not necessary for the LHA to follow up with them. In a few cases, people in quarantine have tested positive for COVID-19 but don’t necessarily have any signs and symptoms.
“Typically, if I am informed the patient is under the care of physician or has been educated to what quarantine means, I wait a week or 2 in cases that I know they’ve been contacted by the state and a physician,” the LHA nurse reported.
Those COVID-19 patients in quarantine who have a physician are instructed by that office regarding what they can or should do, what the quarantine should involve, when to seek emergency help if needed, all in accordance with CDC guidelines. The LHA will usually follow up more frequently with COVID-19 patients who do not have a primary care physician, but not every day.
When the pandemic began, the wait for test results could take as long as 19-days to get back. So, by the time that the LHA received information from the state, those people had already healed. Now, the majority of test results are reported within 24-hours to 3 days, which makes keeping up with patients and tracing easier.
The purpose of calling is not to be a pest to people who are in quarantine, especially those who experiencing COVID-19 symptoms. When the LHA does call patients, the health care professional will “serve as kind of an advocate for patients who need a little bit more assistance and help,” according to the LHA nurse.
“We do want to be a resource. They can call if they have new symptoms, need help obtaining a doctor’s release or how to get prescriptions while in quarantine of if they need food, what you can do. We’ll connect those who genuinely need help with 211, food banks or other resources and help them through the steps of getting help,” the LHA nurse reports.
In some instances, that can include providing employers with information regarding testing results. For instance, some people will continue to test positive for a longer duration than others. According to the CDC, notable is that there have been some reports of prolonged detection of RNA without direct correlation to viral culture.
So, a recovered COVID-19 patient may test positive multiple times even though they haven’t had active COVID-19 for a month or more, according to the LHA nurse.
“I can offer guidance,” the LHA nurse said. “I can help educate the employer and patient. I can send them the CDC link; every single thing I’m doing is based on CDC guidelines.”
When the LHA is contacted regarding a positive COVID-19 patient, Dr. Balkcom calls the state to obtain the patient’s contact information. Then, LHA can contact that individual as needed. If the person cannot be contacted, the LHA nurse will work with the state to try to obtain better contact information.
For instance, the information reported to the state was only a Post Office box and a phone number. Sometimes, numbers aren’t working or current. Sometimes, the number is correct but the person doesn’t answer, because it’s a stranger’s number. Officials keep trying. Sometimes, they mail letters.
Officials have to be careful in any messages left or sent to protect the patient’s confidentiality. If all routes to contact the person go unanswered, someone may be sent to make contact with the individual if there is a concern.
Patients, either through their doctor, the medical facility or otherwise, may be given the number of the LHA so they can talk to the nurse if they have any needs that aren’t being met that the individual’s PCP cannot provide. The LHA can also help them in figuring the needed length of quarantine or isolation, based on their symptoms and CDC guidelines, so they’ll know when they can leave their home.
Another part of the LHA’s job is to try to identify potential hotspots in the community, then providing businesses and facilities with guidance about infection control procedures and policies that, when implemented, can help with disinfection. This can include things like shutting down break rooms and reducing points of contact, and contact tracing if employees get sick, not necessarily with COVID-19. The LHA can help provide tips for preventative infection control.
A COVID-19 patient is considered recovered and OK, even if he/she tested positive, if the individual has gone 72 hours with symptom resolution. That is the person no longer experiences overwhelming fatigue, fever or other acute symptoms. That’s not to say the person doesn’t have some less acute symptoms still, as a residual cough could last up to months later. That just means, to be recovered, the individual has gone 72 hours without aid of any kind of medicine or fever, has improved respiratory symptoms, and 10 days have passed since the individual’s first appeared.
Often times if the state has not gotten around to collecting trace information from the positive COVID-19 patient, the LHA has the ability to it and report the information collected to the state.
“I’m here when they need me. I can do initial tracing if I need to, if it’s not already done. If I notice that, I can work on that from here, then contact them. State and I work together,” the LHA nurse said.
That is the time-based strategy. There’s also a test-based strategy. Guidelines may be found on the CDC website regarding when it’s OK to leave isolation after having COVID-19 or being exposed to someone who tested positive.
State, Local Information Sharing
A number of variables factor into who reports positive test results and patient recoveries when, which can sometimes mean local reports don’t always match state reports.
For instance, the Texas Department of State Health Services/Health and Human Services COVID-19 Dashboard on June 17 showed 44 total cases of COVID-19 since March, 22 active cases and 22 patient recoveries in Hopkins County. Local emergency management officials and Hopkins County Hospital District/EMS, however, on June 17 reported only 43 cases, including 15 recoveries.
Local emergency management and the LHA aren’t able to report any new numbers or information until the state officially reports it to them, according to the LHA.
“There’s a proper chain to go through. We get in trouble if we release it before they make it official. We do everything we can to abide by the rules that we have to follow. We can’t release information until notified by state,” the LHA nurse said.
The process starts with a person having a test either at a mobile collection site, hospital, clinic, physicians office or other private facility after exhibiting symptoms or being in exposed to someone who has COVID-19. When a positive result is returned, if the test wasn’t conducted by the state, the physician or health professional sends the information to DSHS. The patient is notified, as is the local emergency management coordinator. The LHA also receives a call with the information.
While authorities in some areas have opted to release demographics and statistical information to the public, Hopkins County does not. The state cautioned the LHA and emergency management officials to be careful not to violate patients’ privacy rights. As a rule of thumb, they were advised that if any information released can be used to trace the case back to the patient doing so violates the patient’s rights, according to the LHA nurse.
In small communities, providing zip codes, whether the person is male or female and/or the individual’s age could potentially do just that. It could also incite public concern or panic for that area, or even result in bullying or other negative response toward the COVID-19 patients and their families.
“The second part of that is that nobody can prove it would help anything, but it might create hysteria, which does not help. People should take the same precautions no matter the zip codes and age ranges,” the LHA nurse reported.
The LHA reminds that because COVID-19 is prevalent, it is still important for people to take infection control measures in Hopkins County, especially if those who may be immunocompromised. No matter what age or zip code someone lives in, all can potentially be infected or be infectors, according to the LHA nurse.
“The thing with this virus is that it knows no age discrimination. It can affect newborn to 100. We understand why people want to know ages, but it doesn’t serve any definitive purpose. If it would help our community, we would release it,” the LHA nurse said.
Once a person has met criteria to be considered recovered, with doctor approval, the information is sent to the state. Once the state health agency completes their portion of the process, the LHA is notified that the case is officially cleared as a recovery. Only then are local officials allowed to report recoveries.
Over the last couple of weeks, additional cases and recoveries for Hopkins County were posted on the DSHS/HHS dashboard before local officials received official notification regarding the additional cases.
“That’s frustrating. We’ll see that too, incidences of higher numbers or lower numbers, that don’t match,” the LHA nurse reported.
The LHA nurse is frequently checking those numbers to be sure all cases are counted once only. After Hopkins County officials reported the most new COVID-19 cases in a single day. However, after closer examination by the LHA, one of the 10 cases was discovered to have been recorded twice.
Overall, the LHA works in conjunction with other health and emergency officials during the pandemic to see that as many of the COVID-19 patients health and other needs are met.
COVID-19 patients who have questions or concerns or those seeking clarification related to COVID-19, including symptoms may contact the LHA at 903-440-5902.