Hopkins County EMS has earned the American Heart Association’s Mission: Lifeline EMS gold plus recognition, according to Hopkins County EMS Director of services Brent Smith.
The Mission: Lifeline EMS Recognition program is “designed to showcase Emergency Medical Service organizations across the nation for excellent STEMI care,” according to the AHA website.
A STEMI is the term cardiologists use to describe a classic heart attack. It is one type of myocardial infarction in which a part of the heart muscle, the myocardium, has died due to the obstruction of blood supply to the area.
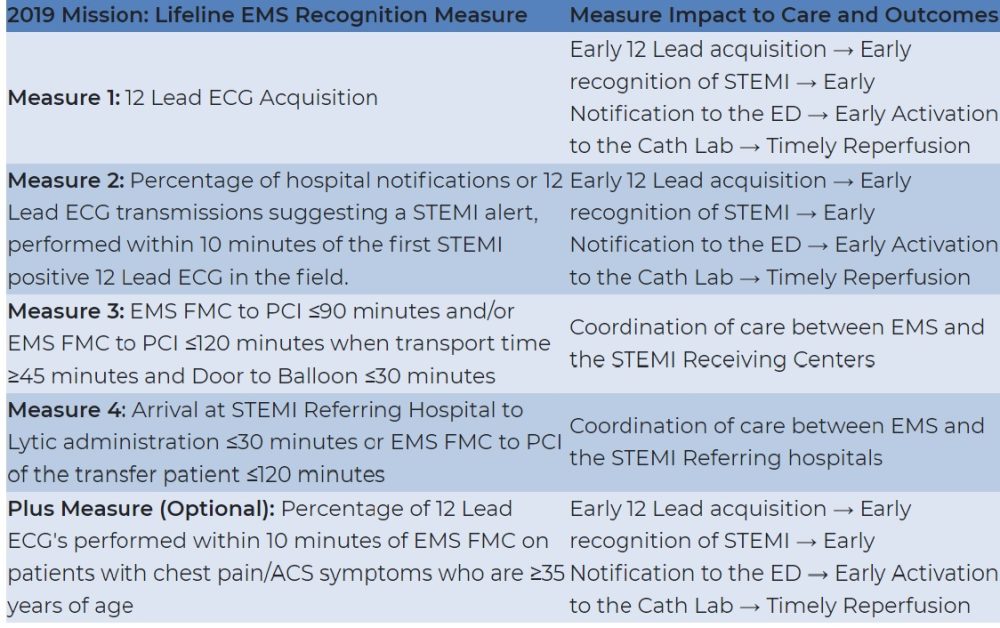
The AHA recognition is earned based on field data and tallies of certain patient reports and medical responses.
Hopkins County EMS has completed the required information to compete in the program since 2015; the data is based on the calendar year, with all data reflected in this award from calendar year 2018.
“This will be the third year in a row we’ve gotten gold plus award, which is the highest award. We got the Gold Award in 2016 and we got the silver award in 2015” said Brent Smith, director of Hopkins County EMS services.
For the award, the AHA looks at four core EMS measures. There are also four optional reporting measures in which EMS services can also submit data for AHA to consider, according to Smith.
One core measure is the percent of patients over 35 years of age who receive a 12-lead by EMS. This is how many people reporting chest pain are checked on a cardiac monitor using a 12-lead, Smith said.
Another asks the percent of patients with 12-leads that show a STEMI, “a ST-segment elevation myocardial infarction,” was performed in the first 10 minutes on scene.
Smith said EMS has put procedures in place to speed up the process described in that core EMS measure.
Core value three asks the percent of patients who had a STEMI resolved in a Cath Lab within 90 minutes of first EMS contact. From the time EMS shows up on a call in which a patient is reported to have chest pain, and reports they are with the patient, that 90 minutes begins, Smith noted.
Hopkins County EMS received 95.28 percent on all three core measures the first quarter, and 100 percent the second, third and fourth quarters of 2018, Smith said.
“I am very proud of those statistics. That’s pretty rock solid across the measures,” he said.
He credited team effort, a lot of education and critical steps taken. He said the Cath Lab and ER staff too are to be credited for their roles as well.
“When we call a STEMI in the field, we notify the hospital as soon as we know about it. We transmit that 12-lead to the hospital so they can confirm. They activate the Cath Lab team and the doctor to come in, if they are not already here [at the hospital]. So, they’ve got to arrive here, the patient has to get here and everything has to flow, where they do everything – shave parts, stick needles in you, put the cath in you – and have it done within 90 minutes, and that’s from the time we arrive at your house. Sometimes, geography is against us, but I will tell you three of our STEMIs were out of Franklin County. That’s a lot of ground to cover in 90 minutes, to where you’re no longer losing a heart muscle because they crossed the legion in 90 minutes,” Smith explained.
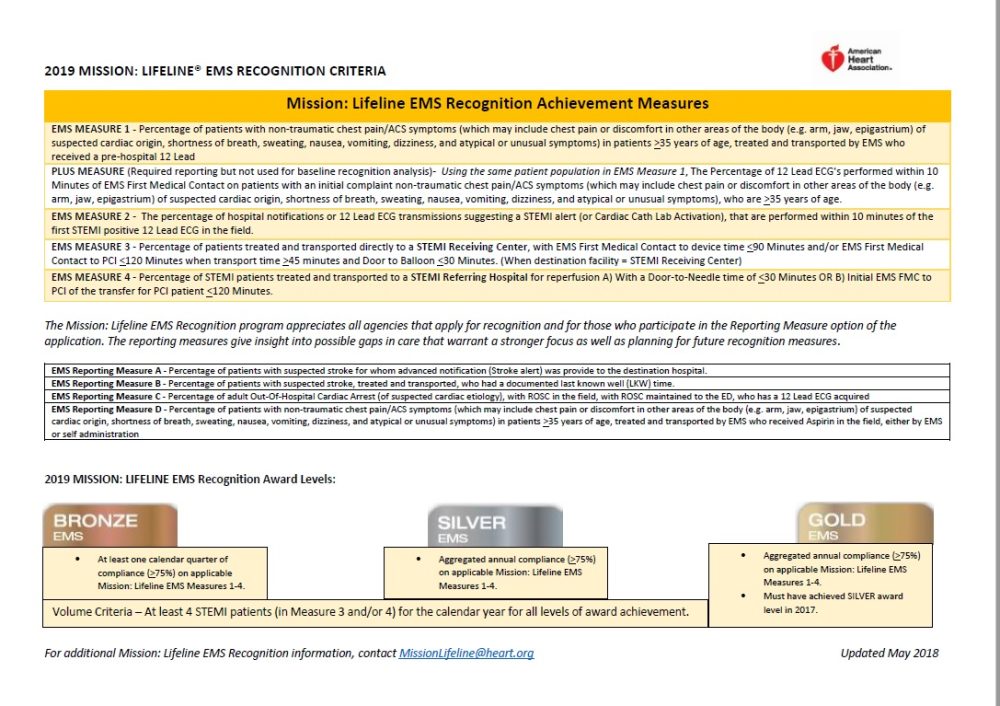
In addition to the core EMS measures, there are also four optional reporting measures, added by AHA a year ago, which EMS services can also submit information on to count in their rating, Smith said.
Optional reporting measures are designed to “give insight into possible gaps in care that warrant a stronger focus as well as planning for future recognition measures,” according to AHA.
Hopkins County EMS only reported on two of the measures the first year, because the data was not at that time being captured in the EMS reporting system,. However, for 2018, the service reported on all measures. Not many do all optional measures, Smith noted.
For the first optional measure, percent of patients with suspected stroke with pre-hospital notification, HCEMS scores 25 percent. Smith said EMS personnel notifythe hospital of a “code stroke” just as they would for a STEMI. Then, upon arrival at the hospital, the doctor does a quick assessment and the patient is taken directly to CT, bypassing an ER bed. With the hospital moving to the stroke center certification, the hospital staff is “on the clock the whole time.”
Smith credited the lower rating on this measure is due largely to the fact that EMS personnel weren’t documenting when they called a code stroke that they notified the hospital. EMS notifies the hospital every time they are bringing a patient in, what they are being brought in for, the EMS services director reports.
On the second optional measure, percent of patients with suspected stroke with documented LKW (last known well time), EMS scored 86 percent. Smith said the results in this measure for 2019 will be 100 percent. That is now a mandatory part of EMS’ patient care reports; the form is set up so that the EMS worker can’t move past the scene on the form until they’ve documented last known well time, he explained.
On optional measure three, percent of out-of-hospital cardiac arrests with ROSC (return of spontaneous circulation), Hopkins County EMS scored 32 percent. The hearts of patients in this category had completely stopped and the patient was revived prior to arrival.
“That number is a little bit low. It goes back to our documentation of capturing that information. I pretty solid say we run more like 40 percent, but 32 percent is what I could back up with paperwork. Before we started with the LUCAS devices our 32 percent was hovering around 14 percent. That’s the difference those machines have really made,” Smith told the hospital board members
For optional measure four, percent of chest pain patients who received aspirin in the field, HCEMS rated 61 percent. Again, Smith cited documentation as contribution to this number. If a patient has already taken aspirin, it counts toward the measure, if documented. The EMS service’s documentation form did not ask the paramedic that question. The 61 percent reflects the number of all chest patients they responded to who received aspirin. He said he suspected some had already received aspirin, and EMS staff are now asking and documenting that too.
“We have some room to work on optional measures. I think the common denominator is documentation. But I feel very proud of what all the field staff are doing, with these measures as well,” Smith said.